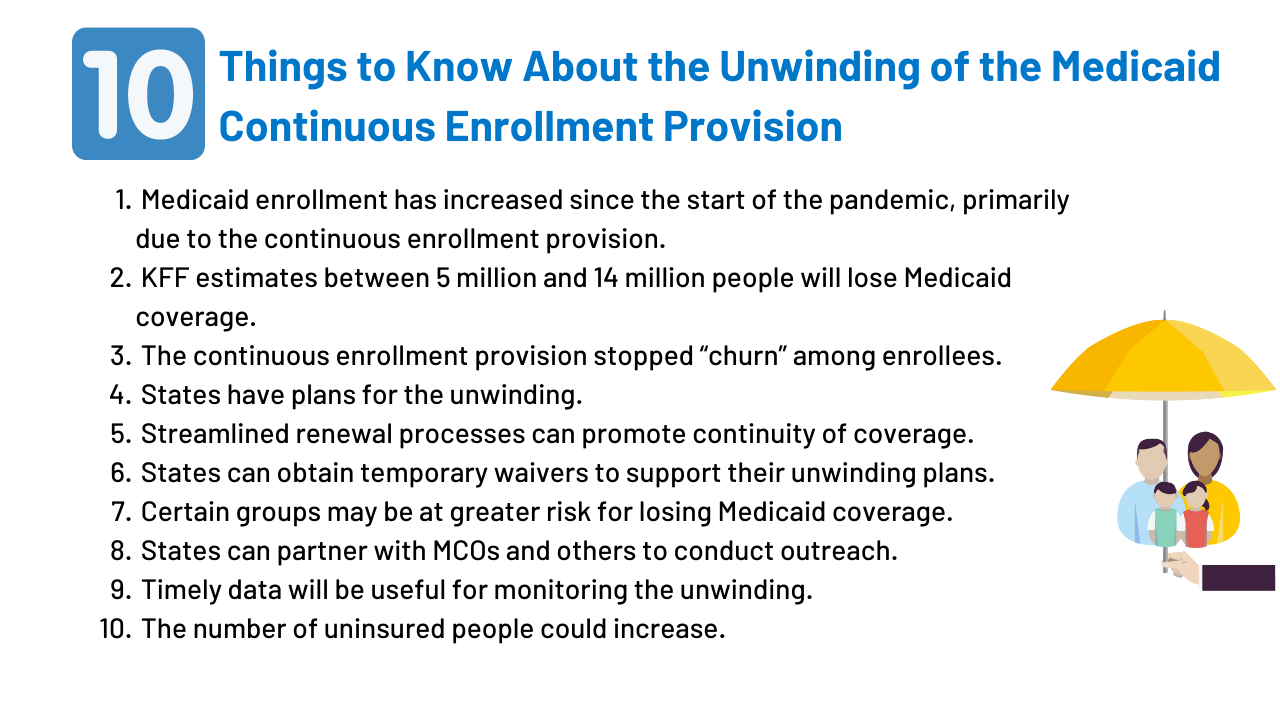
10 Things to Know About the Unwinding of the Medicaid Continuous Enrollment Provision
Note: This brief was updated April 5, 2023, to include more recent and additional data.
- Medicaid enrollment has increased since the start of the pandemic, primarily due to the continuous enrollment provision.
- KFF estimates that between 5 million and 14 million people will lose Medicaid coverage during the unwinding of the continuous enrollment provision.
- The Medicaid continuous enrollment provision has stopped “churn” among Medicaid enrollees.
- States have developed plans for how they will approach the unwinding of the continuous enrollment provision.
- Maximizing streamlined renewal processes can promote continuity of coverage as states begin to unwind the continuous enrollment provision.
- States can obtain temporary waivers to pursue strategies to support their unwinding plans.
- Certain groups may be at greater risk for losing Medicaid coverage during the unwinding period.
- States can partner with MCOs, community health centers, and other partners to conduct outreach.
- Timely data on disenrollments and other metrics will be useful for monitoring how the unwinding is proceeding.
- The number of people without health insurance could increase if people who lose Medicaid coverage are unable to transition to other coverage.
At the start of the pandemic, Congress enacted the Families First Coronavirus Response Act (FFCRA), which included a requirement that Medicaid programs keep people continuously enrolled through the end of the COVID-19 public health emergency (PHE), in exchange for enhanced federal funding. As part of the Consolidated Appropriations Act, 2023, signed into law on December 29, 2022, Congress delinked the continuous enrollment provision from the PHE, ending continuous enrollment on March 31, 2023. The CAA also phases down the enhanced federal Medicaid matching funds through December 2023. Primarily due to the continuous enrollment provision, Medicaid enrollment has grown substantially compared to before the pandemic and the uninsured rate has dropped. But, as states resume disenrollments following the end of the continuous enrollment provision, millions of people could lose coverage and that could reverse recent gains in coverage. States can resume disenrollments beginning in April but must meet certain requirements to be eligible for enhanced federal funding during the unwinding.
This brief describes 10 key points about the unwinding of the Medicaid continuous enrollment provision, highlighting data and analyses that can inform the unwinding process as well as legislation and guidance issued by the Centers for Medicare and Medicaid Services (CMS) that lay out the rules states must follow during the unwinding period and the flexibilities available to them.
1. Medicaid enrollment has increased since the start of the pandemic, primarily due to the continuous enrollment provision.
The Consolidated Appropriations Act, 2023 decouples the Medicaid continuous enrollment provision from the PHE and terminates this provision on March 31, 2023. Starting April 1, 2023, states can resume Medicaid disenrollments. States will be eligible for the phase-down of the enhanced FMAP (6.2 percentage points through March 2023; 5 percentage points through June 2023; 2.5 percentage points through September 2023 and 1.5 percentage points through December 2023) if they comply with certain rules. They cannot restrict eligibility standards, methodologies, and procedures and cannot increase premiums as required in FFCRA. Further, states must also comply with federal rules about conducting renewals. Lastly, states are required to maintain up to date contact information and attempt to contact enrollees prior to disenrollment when mail is returned.
2. KFF estimates that between 5 million and 14 million people will lose Medicaid coverage during the unwinding of the continuous enrollment provision.
While the number of Medicaid enrollees who may be disenrolled during the unwinding period is highly uncertain, KFF estimates that between 5.3 million and 14.2 million people will lose Medicaid coverage during the 12-month unwinding period reflecting a 5{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} and 13{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} decline in enrollment (Figure 2). These projected coverage losses are consistent with, though a bit lower than, estimates from the Department of Health and Human Services (HHS) suggesting that as many as 15 million people will be disenrolled, including 6.8 million who will likely still be eligible. While the share of individuals disenrolled across states will vary due to differences in how states prioritize renewals, it is expected that the groups that experienced the most growth due to the continuous enrollment provision—ACA expansion adults, other adults, and children—will experience the largest enrollment declines. Efforts to conduct outreach, education and provide enrollment assistance can help ensure that those who remain eligible for Medicaid are able to retain coverage and those who are no longer eligible can transition to other sources of coverage.
3. The Medicaid continuous enrollment provision has stopped “churn” among Medicaid enrollees.
The temporary loss of Medicaid coverage in which enrollees disenroll and then re-enroll within a short period of time, often referred to as “churn,” occurs for a several reasons. Enrollees may experience short-term changes in income or circumstances that make them temporarily ineligible. Alternatively, some people who remain eligible may face barriers to maintaining coverage due to renewal processes and periodic eligibility checks. Eligible individuals are at risk for losing coverage if they do not receive or understand notices or forms requesting additional information to verify eligibility or do not respond to requests within required timeframes. Churn can result in access barriers as well as additional administrative costs. Estimates indicate that among full-benefit beneficiaries enrolled at any point in 2018, 10.3{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} had a gap in coverage of less than a year (Figure 3). About 4.2{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} were disenrolled and then re-enrolled within three months and 6.9{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} within six months. Another analysis examining a cohort of children newly enrolled in Medicaid in July 2017 found that churn rates more than doubled following annual renewal, signaling that many eligible children lose coverage at renewal. By halting disenrollment during the PHE, the continuous enrollment provision has also halted this churning among Medicaid enrollees.
4. States have developed plans for how they will approach the unwinding of the continuous enrollment provision.
CMS requires states to develop operational plans for how they will approach the unwinding process. These plans must describe how the state will prioritize renewals, how long the state plans to take to complete the renewals as well as the processes and strategies the state is considering or has adopted to reduce inappropriate coverage loss during the unwinding period. An Informational Bulletin (CIB) posted on January 5, 2023 included timelines for states to submit a renewal redistribution plan.
According to a KFF survey conducted in January 2023, states have taken a variety of steps to prepare for the end of the continuous enrollment provision (Figure 4). Under CMS guidance, states had the option to start the unwinding period by initiating the first batch of renewals in February, March, or April. Eight states started the process in February, another 15 started in March, and 28 states began in April. Most states (43) said they plan to take 12-14 months to complete all renewals (the remaining eight states said they planned to take less than 12 months to complete renewals). All states indicated they had taken steps to update enrollee contact information during the past year and nearly three-quarters of states (37) were planning to follow up with enrollees before terminating coverage. As of March 13, 2023, 26 states had posted their renewal redistribution plan, which had to be submitted to CMS by February 15, 2023 for most states. How states approach the unwinding process will have implications for the ability of eligible individuals to retain coverage and those who are no longer eligible to transition to other coverage. Outcomes will differ across states as they make different choices and face challenges balancing workforce capacity, fiscal pressures, and the volume of work.
5. Maximizing streamlined renewal processes can promote continuity of coverage as states begin to unwind the continuous enrollment provision.
Under the ACA, states must seek to complete administrative (or “ex parte”) renewals by verifying ongoing eligibility through available data sources, such as state wage databases, before sending a renewal form or requesting documentation from an enrollee. Some states suspended renewals as they implemented the continuous enrollment provision and made other COVID-related adjustments to operations. Completing renewals by checking electronic data sources to verify ongoing eligibility reduces the burden on enrollees to maintain coverage. While 30 states have taken action in the past year to increase ex parte renewal rates, in many states, the share of renewals completed on an ex parte basis is low. Of the 43 states processing ex parte renewals for MAGI groups (people whose eligibility is based on modified adjusted gross income), 18 states report completing 50{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} or more of renewals using ex parte processes. Twenty states complete less than 50{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of renewals on an ex parte basis, including 11 states where less than 25{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of renewals are completed using ex parte processes (Figure 5). The number of states reporting they complete more than 50{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of renewals using ex parte processes for non-MAGI groups (people whose eligibility is based on being over age 65 or having a disability) is even lower at 6.
As states begin to unwind the continuous enrollment provision, there are opportunities to promote continuity of coverage among enrollees who remain eligible by increasing the share of renewals completed using ex parte processes and taking other steps to streamline renewal processes (which will also tend to increase enrollment and spending). CMS guidance notes that states can increase the share of ex parte renewals they complete without having to follow up with the enrollee by expanding the data sources they use to verify ongoing eligibility. However, when states do need to follow up with enrollees to obtain additional information to confirm ongoing eligibility, they can facilitate receipt of that information by allowing enrollees to submit information by mail, in person, over the phone, and online. While nearly all states accept information in-person (51 states) and by mail (50 states), slightly fewer provide options for individuals to submit information online (48 states) or over the phone (46 states).
A proposed rule, released on September 7, 2022, seeks to streamline enrollment and renewal processes in the future by applying the same rules for MAGI and non-MAGI populations, including limiting renewals to once per year, prohibiting in-person interviews and requiring the use of prepopulated renewal forms. Overall, every state has taken at least one action to align renewal processes for non-MAGI populations with those for MAGI populations, including 45 states that have eliminated in-person interviews, 42 states that limit renewals to once per year, and 33 states that send pre-populated renewal forms.
(Back to top)
6. States can obtain temporary waivers to pursue strategies to support their unwinding plans.
As states prepare to complete redeterminations for all Medicaid enrollees, many may face significant operational challenges related to staffing shortages and outdated systems. To reduce the administrative burden on states, CMS announced the availability of temporary waivers through Section 1902(e)(14)(A) of the Social Security Act. These waivers will be available on a time-limited basis and will enable states to facilitate the renewal process for certain enrollees with the goal minimizing procedural terminations. As of February 24, 2023, CMS had approved a total of 163 waivers for 43 states (Figure 6). These waivers include strategies allowing states to: renew enrollee coverage based on SNAP and/or TANF eligibility; allow for ex parte renewals of individuals with zero income verified within the past 12 months; allow for renewals of individuals whose assets cannot be verified through the asset verification system (AVS); partner with managed care organizations (MCOs), enrollment brokers, or use the National Change of Address (NCOA) database or US postal service (USPS) returned mail to update enrollee contact information; extend automatic enrollment in MCO plans up to 120 days; and extend the timeframe for fair hearing requests.
7. Certain groups may be at greater risk for losing Medicaid coverage during the unwinding period.
As states resume redeterminations and disenrollments, certain individuals, including people who have moved, immigrants and people with limited English proficiency (LEP), and people with disabilities, will be at increased risk of losing Medicaid coverage or experiencing a gap in coverage due to barriers completing the renewal process, even if they remain eligible for coverage. Enrollees who have moved may not receive important renewal and other notices, especially if they have not updated their contact information with the state Medicaid agency. In 2020, one in ten Medicaid enrollees moved in-state and while shares of Medicaid enrollees moving within a state has trended downward in recent years, those trends could have changed in 2021 and 2022.
A recent analysis of churn rates among children found that while churn rates increased among children of all racial and ethnic groups, the increase was largest for Hispanic children, suggesting they face greater barriers to maintaining coverage. Additionally, people with LEP and people with disabilities are more likely to encounter challenges due to language and other barriers accessing information in needed formats. An analysis of state Medicaid websites found that while a majority of states translate their online application landing page or PDF application into other languages, most only provide Spanish translations (Figure 7). That same analysis revealed that a majority of states provide general information about reasonable modifications and teletypewriter (TTY) numbers on or within one click of their homepage or online application landing page (Figure 8), but fewer states provide information on how to access applications in large print or Braille or how to access American Sign Language interpreters.
CMS guidance about the unwinding of the continuous enrollment provision stresses the importance of conducting outreach to enrollees to update contact information and provides strategies for partnering with other organizations to increase the likelihood that enrollee addresses and phone numbers are up to date. CMS guidance also outlines specific steps states can take, including ensuring accessibility of forms and notices for people with LEP and people with disabilities and reviewing communications strategies to ensure accessibility of information. Ensuring accessibility of information, forms, and assistance will be key for preventing coverage losses and gaps among these individuals.
(Back to top)
8. States can partner with MCOs, community health centers, and other partners to conduct outreach.
States can collaborate with health plans and community organizations to conduct outreach to enrollees about the need to complete their annual renewal during the unwinding period. CMS has issued specific guidance allowing states to permit MCOs to update enrollee contact information and facilitate continued enrollment. According to a survey of non-profit, safety net health plans that participate in Medicaid, a majority of responding MCOs reported that they are sending updated member contact information to their state. Additionally, nearly two-thirds of states (33) are planning to send MCOs advance lists of members for whom the state is initiating the renewal process and about half will send lists of members who have not submitted renewal forms and are at risk of losing coverage or who have been disenrolled indicating whether the member was determined no longer eligible or disenrolled for paperwork reasons (Figure 9).
States can also work with community health centers, navigators and other assister programs, and community-based organizations to provide information to enrollees and assist them with updating contact information, completing the Medicaid renewal process, and transitioning to other coverage if they are no longer eligible. A survey of health centers conducted in late 2021 found that nearly 50{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of responding health centers reported they have or plan to reach out to their Medicaid patients with reminders to renew their coverage and to schedule appointments to assist them with renewing coverage. Similarly, a survey of Marketplace assister programs found that assister programs were planning a variety of outreach efforts, such as public education events and targeted outreach in low-income communities, to raise consumer awareness about the end of the continuous enrollment provision. Additionally, nearly six in ten assister programs said they had proactively reached out to their state to explore ways to help consumers; supported the state sharing contact information with them on individuals who need to renew their Medicaid coverage; and were planning to recontact Medicaid clients to update their contact information.
(Back to top)
9. Timely data on disenrollments and other metrics will be useful for monitoring how the unwinding is proceeding.
On January 5, 2023, CMS released an Informational Bulletin that included timelines for states to submit a renewal redistribution plan (discussed above), system readiness plans and results, and baseline unwinding data based on when states plan to begin renewals. These reporting requirements were part of a broad set of CMS guidance documents issued over the past several months. For system readiness reporting, states are required to demonstrate that their eligibility systems for processing renewals are functioning correctly, particularly since states have not been conducting normal renewals while the continuous enrollment provision has been in effect. For enrollment reporting, states will provide baseline data at the start of the unwinding period related to applications, enrollment, estimated timeframe for completing initiated renewals, and fair hearings, and then states will submit monthly reports that will be used to monitor these metrics throughout the unwinding period (Figure 10). The recent CIB notes that CMS is expected to issue guidance to address how new reporting requirements (discussed below) may intersect with the requirements described in prior CMS guidance.
The recently enacted Consolidated Appropriations Act includes additional reporting requirements for states and imposes penalties in the form of reduced federal matching payments for states that do not comply. These enhanced reporting metrics require states to report the total number of individuals renewed and those renewed on an ex parte basis, break out Medicaid terminations for children’s coverage and pregnancy-related coverage, report the number of individuals whose coverage was terminated for procedural reasons, including breakouts for children’s coverage and pregnancy-related coverage, and report total call center volume, average wait time, and average abandonment rate. States are also required to report on transitions to separate CHIP programs and to Marketplace or Basic Health Program coverage (Figure 10). Importantly, the legislation requires that CMS make these reports publicly available. Nearly half of states (24) indicated they plan to publish some unwinding data on their websites, while 21 states had not yet made a decision about posting the data. States that fail to comply with these reporting requirements face a reduction in federal medical assistance percentage (FMAP) of up to one percentage point for the quarter in which the requirements are not met. If CMS determines a state is out of compliance with any applicable redetermination and reporting requirements, it can require the state to submit a corrective action plan and can require the state to suspend all or some terminations due to procedural reasons until the state takes appropriate corrective action.
Collectively, these metrics are designed to demonstrate states’ progress towards restoring timely application processing and initiating and completing renewals of eligibility for all Medicaid and CHIP enrollees and can assist with monitoring the unwinding process to identify problems as they occur. However, while the new data reporting requirements are useful, they will not provide a complete picture of how the unwinding is proceeding and whether certain groups face barriers to maintaining coverage. To fully assess the impact of the unwinding will require broader outcome measures, such as continuity of coverage across Medicaid, CHIP, Marketplace, and employer coverage, gaps in coverage over time, and increases in the number of the uninsured, data that will not be available in the short-term.
10. The number of people without health insurance could increase if people who lose Medicaid coverage are unable to transition to other coverage.
The share of people who lack health insurance coverage dropped to 8.6{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} in 2021, matching the historic low in 2016, largely because of increases in Medicaid coverage, and to a lesser extent, increases in Marketplace coverage. However, as states resume Medicaid disenrollments, these coverage gains could be reversed. CMS guidance provides a roadmap for states to streamline processes and implement other strategies to reduce the number of people who lose coverage even though they remain eligible. However, there will also be current enrollees who are determined to be no longer be eligible for Medicaid, but who may be eligible for ACA marketplace or other coverage. A MACPAC analysis examined coverage transitions for adults and children who were disenrolled from Medicaid or separate CHIP (S-CHIP) and found that very few adults or children transitioned to federal Marketplace coverage, only 21{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of children transitioned from Medicaid to S-CHIP, while 47{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} of children transitioned from S-CHIP to Medicaid (Figure 11).
A KFF analysis revealed that among people disenrolling from Medicaid, roughly two-thirds (65{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7}) had a period of uninsurance in the year following dise0nrollment and only 26{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} enrolled in another source of coverage for the full year following disenrollment (Figure 12). Together, these findings suggest that individuals face barriers moving from Medicaid to other coverage programs, including S-CHIP. Simplifying those transitions to reduce the barriers people face could help ensure people who are no longer eligible for Medicaid do not become uninsured. Importantly, these findings also show that large shares of enrollees (41{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7} in the KFF analysis) reenroll in Medicaid after a period of time, and many after a period of uninsurance. Reducing the number of people who lose coverage for procedural reasons even though they remain eligible can also help to reduce the number of people who become uninsured.
The proposed eligibility and enrollment rule aims to smooth transitions between Medicaid and CHIP by requiring the programs to accept eligibility determinations from the other program, to develop procedures for electronically transferring account information, and to provide combined notices. States can also consider sharing information on consumers losing Medicaid who may be eligible for Marketplace coverage with Marketplace assister programs; however, in a 2022 survey, few assister programs (29{a652ac39cb023ff8fd1cc85f4393f5b1bb70bf2f880b7bee35f712e4bd8633f7}) expected states to provide this information although nearly half were unsure of their state’s plans.
(Back to top)




:quality(70)/d1hfln2sfez66z.cloudfront.net/02-02-2023/t_832fc9813d3741189856dfd7da126358_name_Car_Insurance_Increase_transfer_frame_627.jpeg)